Our Welcoming Reception & 1st Waiting Area
Our Ground Floor Operatory
Our Ground Floor Operatory
Our Laboratory
Our Display Area With Updated Oral Hygiene Measures
Our First Floor Operatory
Our First Floor Operatory
Tooth Removal
Oral and Maxillofacial Surgery is a surgery to correct a wide spectrum of diseases, injuries and defects in the head, neck, face, jaws and the hard and soft tissues of the oral and maxillofacial region. It is a recognized international dental specialty, which requires a minimum length of formation of 5 years for a basic dental training and 3 years for a basic medical and dental training, in India.
Oral and maxillofacial surgeons are trained to treat problems such as the extraction of wisdom teeth, misaligned jaws, tumors and cysts of the jaw and mouth and to perform dental implant surgery. They are also trained to administer anesthesia, and provide care in an office setting. Oral and Maxillofacial Surgeons (OMFS) frequently work alongside other specialists including Dentists, Orthodontists, Prosthodontists, Radiologists, Pathologists, Oncologists, ENT surgeons, Neurosurgeons, Plastic surgeons and professionals allied to medicine.
FREQUENTLY ASKED QUESTION
- Q: What can an Oral and Maxillofacial surgeon do?
- Q: What is impacted tooth and why am I in need to go to an Oral and Maxillofacial Surgeon for its removal?
- Q: What kind of a procedure is it?
- Q: Whether I am in need of a hospital stay for this?
- Q: How much time will this procedure take ?
- Q: Will I be facing any complication after the procedure?
- Q: What about the sutures which has been placed postoperatively?
- Q: What are the instructions I am supposed to follow after this procedure?
- Q: What is Temporomandibular joint disorder (TMJD, TMJ or TMD), or TMJ syndrome?
- Q: How will I know that I am facing TMJ problem?
- Q: What kind of treatment can be given?
- Q: What is Oral Cancer?
- Q: Is it very common?
- Q: What are the early warning signs?
- Q: Can I examine myself?
- Q: What are the early clinical indicators?
- Q: Can Oral Cancer be cured?
- Q: How to avoid Oral Cancer?
- Q: What is orthognathic surgery?
- Q: Who Needs Orthognathic Surgery?
- Q: What is Trauma?
- Q: Who is a trauma patient?
- Q: What is a Trauma Center?
- Q: What do the different levels of trauma centers mean?
- Q: How come I know that I need treatment from oral and maxillofacial surgeon?
- Q: What procedures are performed?
- Q: Who gets facial reconstruction following trauma?
- Q: How are the outcomes of reconstruction following trauma?
- Q: Does insurance cover it?
Still have questions?
Ask us for more information.
Q: What an Oral and Maxillofacial surgeon can do?
A: These surgeons are usually specialized in diagnosis and treatment of diseases affecting the oral (mouth) and maxillofacial (face and neck) regions, including the following:
- Oral and Dentoalveolar Surgery (removal of impacted and buried teeth, cysts, etc.).
- Preprosthetic Surgery (bone augmentation).
- Dental implant surgery and associated bone grafting (to replace missing teeth or stabilise dentures; rehabilitation of patients having undergone surgery for tumours; to retain facial prostheses).
- Orthognathic surgery (dentofacial deformities for esthetic and functional purpose).
- Facial trauma surgery (facial bone fractures and injuries).
- Surgery of Odontogenic and non-odontogenic Tumors.
- Reconstructive surgery.
- Cleft lip and palate surgery.
- Congenital craniofacial deformities.
- Facial plastic surgery (rhinoplasty, rhytidectomy, blepharoplasty, facial implants, etc.)
- Tempromandibular joint disorders(TMJD).
Q: What is impacted tooth and why am I in need to go to an Oral and Maxillofacial Surgeon for its removal?
A: A tooth is said to be impacted when it does not have enough space for its eruption in your oral cavity. As such any tooth can be impacted but most of the time its your wisdom tooth (3rd molars) which gets impacted.These teeth can cause pain, swelling, infection and various other problems so they need to be removed and your oral and maxillofacial surgeon is specialized in removing such teeth. And we have a highly skilled surgeon Dr. Manjunath Rai for atraumatic removal of this tooth.
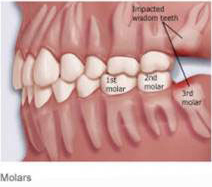
Diagram showing impaction of upper and lower third molars as they are not having enough space to erupt.
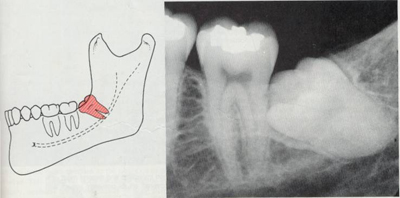
Mesioangular impaction of wisdom tooth
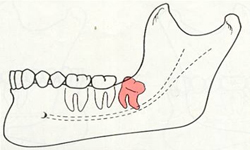
Distoangular impaction of wisdom tooth.
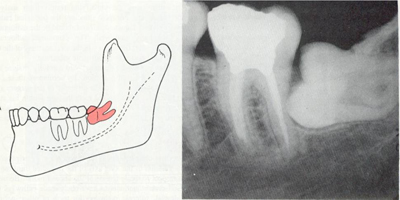
Horizontal impaction of wisdom tooth.
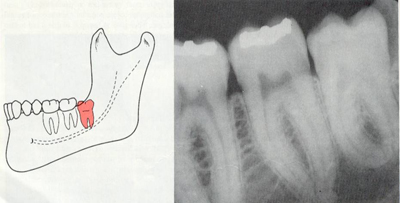
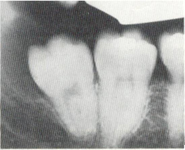
Vertical impaction of wisdom tooth
Q: What kind of procedure it is?
A: This is a minor surgical procedure; most of the time done under local anesthesia after radiographic evaluation. Certain amount of bone has to be removed and tooth is taken out with or without splitting of the tooth. After that suture are given for closure of the soft tissue.
Q: Whether I am in need of a hospital stay for this?
A: No, it is most commonly done procedure on routine outdoor patients.
Q: How much time this procedure will take?
A: Each individual impacted tooth is unique and depending on how it impacted the duration of procedure varies. But most of the time it will take 30-45minutes.
Q: Whether I will be facing any complication after the procedure?
A: You may have minor swelling and pain for few days afterwards ( most of the time it subsides in 3-5 days)Your doctor will be prescribing you painkillers and course of antibiotic. (if at all it is required) But you have to maintain your oral hygiene and you will be on soft and cold diet for few days.
Q: What about the sutures which has been given to me postoperatively?
A: Yah, you have to visit again for its removal afer 5-7days.
Q: what kind of instruction I am supposed to follow after this procedure?
A: The following are the few instructions which you are suppose to follow after procedure:
Care of the Mouth after Local Anesthetic
You had local anesthetic for their dental procedure :
- If the procedure was in the lower jaw... the tongue, teeth, lip and surrounding tissue will be numb or asleep.
- If the procedure was in the upper jaw... the teeth, lip and surrounding tissue will be numb or asleep.
- Please keep the traumatized area as-clean-as possible. A soft wash cloth often works well during healing to aid the process.
- If the swelling re-occurs, we need to see the patient as-soon-as possible. Ice should be administered during the first 24 hours to keep the swelling to a minimum.
- Watch for infection (gum boils) in the area of trauma. If infection is noticed call the office so the patient can be seen as-soon-as possible.
- Maintain a soft diet for two to three days, or until you feel comfortable eating normally again.
- Avoid sweets or foods that are extremely hot or cold.
- If antibiotics or pain medicines are prescribed, be sure to follow the prescription as directed.
- Please do not hesitate to call the office if there are any questions.
- Do not scratch, chew, suck, or rub the lips, tongue, or cheek while they feel numb or asleep.
- Do not rinse the mouth for several hours.
- Do not drink a carbonated beverage (Coke, Sprite, etc.) for the remainder of the day.
- Keep fingers and tongue away from the extraction area.
- Make sure to keep the area clean using soft brushing strokes with a toothbrush.
- Maintain a soft diet for a day or two, or until you feel comfortable eating normally again.
- Avoid strenuous exercise or physical activity for several hours after the extraction.
- Stand in front of a mirror in good light.
- Open your mouth wide. Look for small lumps or swelling, ulcers, a red or white patch.
- If you have dentures, take them out and inspect your mouth.
- Inspect the lips with your mouth both open and closed.
- Stick your tongue out and inspect the margins, as well as below the tongue. If you see something that is unexplained, visit your dentist immediately.
- Avoid bad oral habits like chewing tobacco, gutka and smoking. These bad habits increase your chances of getting oral cancer dramatically.
- Eat a diet rich in fiber, fresh fruits and vegetables, fish and dairy products such as butter, milk etc.
- Visit your dentist twice a year.
- Brush twice a day and maintain good oral hygiene.
Sometimes, you do not understand the effects of local anesthesia, and may chew, scratch, suck the tongue or cheek. These actions can cause minor irritations or they can be severe enough to cause swelling and abrasions to the tissue. Please take care until the anesthetic has worn off. (2-3 hrs generally it takes to wear off its effect) Please do not hesitate to call the office if there are any questions.
Care of the Mouth after Trauma
Care of the Mouth after Extractions
Bleeding
Some bleeding is to be expected. If unusual or sustained bleeding occurs, place cotton gauze firmly over the extraction area and bite down or hold in place for fifteen minutes. This can also be accomplished with a tea bag. Repeat if necessary.
Pain
For discomfort use painkiller as directed. If a medicine was prescribed, then follow the directions on the bottle. Please do not hesitate to contact the office if there are any questions.
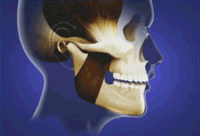
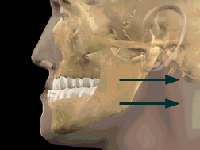
Q: What is Temporomandibular joint disorder (TMJD, TMJ or TMD), or TMJ syndrome?
A: It is an umbrella term covering acute or chronic inflammation of the temporomandibular joint, which connects the lower jaw to the skull. The disorder and resultant dysfunction can result in significant pain and impairment.
The temporomandibular joint is susceptible to all the conditions that affect other joints in the body, including ankylosis, arthritis, trauma, dislocations, developmental anomalies and neoplasia. Although treatment is often similar to other joints in the body, some variations exist
Q: How come I know that I am facing this problem?
A: The presentation of TMJD can be very complex. Often the symptoms will involve more than one of the numerous TMJ components: Muscles, Nerves, Tendons, Ligaments, Bones, Connective Tissue and the Teeth.
Most of the time you will be facing muscular pain and dysfunction of the joint. It may be due to over usage of the muscles e.g. chewing gum continuously, biting habits (fingernails and pencils), grinding habits and clenching habits. And pain can be referred to surrounding soft tissues and to ear. You may face difficulty in opening and closing the mouth and sometimes deviation while opening and closing.
Q: What kind of treatment can be given?
A: Every case is different and treatment depends upon the actual underlying cause of disease. It may be surgical or non surgical.In non surgical methods your doctor can do · Filling or grinding of your tooth which is creating problem · Can prescribe you pain killer· Can provide you some oral appliance to get rid off you from your Para functional habits and to reduce load on your muscles· Can advice you to perform Gentle jaw stretching and relaxation exercises which you can do at homeIn Surgical method your doctor can do Various Surgical procedures from minor to major.•Replacement of the jaw joint(s) or disc(s) with TMJ implants should be considered only as a treatment of last resort.
Q: What is Oral Cancer?
A: Oral Cancer is a disease that starts as an uncontrolled growth of cells in the mouth. It leads to disfigurement of the face, debility of body and eventually death.
Q: Is it very common?
A: Oral Cancer is the most common of cancers in India with as many as 64,460 cases reported each year. That makes it as common as cancer of the lungs, breast or cervix. As much as 7% of all cancer deaths in males 4% in females have been reported to be due to oral cancer. The figure continues to rise rapidly because of bad oral habits such as chewing of gutka, tobacco and smoking among others.
What are the early warning signs?
A: A white or red patch in the mouth or on the tongue, a painless ulcer which doesn't heal for over two weeks, difficulty in eating, drinking and speaking are some of the early signs of oral cancer. If these symptoms appear, you must see your dentist immediately.
Q: Can I examine myself?
A: Yes, you can. In fact it is strongly recommended because early detection can greatly increase the chances of a complete cure.
Q: What are the early clinical indicators?
A: A good dentist is trained to recognize the clinical symptoms of an early oral caner:
Leukoplakia
It is a raised white patch, which is associated with the constant chewing of tobacco and gutka. 2.8% of oral Leukoplakia results in cancerous growths
Oral sub mucous fibrosis
It is the inability to open the mouth and / or a burning sensation which affects 9 per 10,000 Indians.
Lichen Planus
It is a skin affliction occurring in the mouth. It can be caused due to stress and diabetes.
Anemia
It is a deficiency of iron very common in India, which can lead to the development of oral cancer. Q: Can Oral Cancer be cured ?
A: If detected early, oral cancer is curable. The smaller the ulcer or affliction, the better the chances of cure. Treatment involves the surgical removal of the afflicted parts followed by radiation. Chemotherapy is rarely advocated. Cancer of the lip shows 85% cure-rate. Other oral cancers if detected early and treated promptly, may prolong the life of the patients, by as much as 20 years
Q: How to avoid Oral Cancer ?
A: Since oral cancer is very common in India, extra precaution is suggested.
Q: What is Orthognathic surgery?
A: It is surgery related to correction of jaw bones. Orthognathic surgery is needed when jaws don't meet correctly and/or teeth don't seem to fit with jaws. Teeth are straightened with orthodontics and corrective jaw surgery repositions misaligned jaws. This not only improves facial appearance, but also ensures that teeth meet correctly and function properly.
Q: Who Needs Orthognathic Surgery?
A: People who can benefit from orthognathic surgery include those with an improper bite or jaws that are positioned incorrectly. Jaw growth is a gradual process and in some instances, the upper and lower jaws may grow at different rates. The result can be a host of problems that can affect chewing function, speech, long-term oral health and appearance. Injury to the jaw and birth defects can also affect jaw alignment. And Orthodontics alone can not correct bite problems.
Q: What is Trauma?
A: Trauma is a surgical disease demanding surgical leadership.
Q: Who is a trauma patient?
A: The Ohio Revised Code (ORC) 4765.01 defines a trauma patients as someone with a significant risk of loss of life, limb, significant permanent disfigurement or disability caused by blunt or penetrating injury.
Q: What is a Trauma Center?
A: A Trauma Center is a healthcare facility that has established an organized operational structure that facilitates and improves care of the injured patient.
Q: What do the different levels of trauma centers mean?
A: American College of Surgeons definitions:
A Level 1 facility is a regional resource trauma center that is a tertiary care facility central to the trauma care system. This facility must be capable of providing leadership and total care for every aspect of injury, from prevention through rehabilitation.
A Level 2 facility is expected to provide initial definitive trauma care, regardless of injury severity. However, the Level 2 center may not be able to provide the same comprehensive care as a Level 1 center.
A Level 3 facility provides advanced trauma life support (ATLS) prior to transfering the patient in areas where no higher level of care is available.
A Level 4 facility must have a relationship with a Level 1, 2 or 3 trauma center. Patients are stablized and transfered to a higher level facility for trauma care and for the treatment as a whole you need specialist like to treat trauma in oral and maxillofacial region you need oral and maxillofacial surgeon
Q: How come I know that I need treatment from oral and maxillofacial surgeon?
A: If you’ve experienced facial trauma, or have lasting deformity following trauma, you may be a candidate for treatment from oral and maxillofacial surgeon.
Q: What procedures are performed?
A: A few of the procedures performed include repair of complex cut and injuries of the face and deeper tissues, including the eyelids, brows, nose, ears, lips, mouth and cheeks. Broken bone repairs include fractures of the upper and lower jaws, nose, eye sockets, cheekbones and forehead bones. Procedures are designed to maximize functional and cosmetic outcomes.
Q: Who gets facial reconstruction following trauma?
A: Facial trauma occurs across all ages and all walks of life. Severe cuts, broken facial bones and other injuries are all subject to repair and reconstruction. The best way to prevent post-traumatic facial deformities is to obtain the appropriate treatment at the time of the injury.
Q: How are the outcomes of reconstruction following trauma?
A: At first glance, facial trauma can appear complex and difficult to treat. The actual treatment involves a colaboration of many smaller procedures that are commonplace in maxillofacial injuries. Adhering to a treatment protocol and treating each fracture as a unit enables the surgeon to obtain reproducibly good results.
Q: Does insurance cover it?
A: Facial trauma surgery and reconstruction is typically covered by insurance.
